Abstract
Background: Malnutrition is a common condition observed in children with thalassemia. However, the prevalence of malnutrition, alterations of plasma metabolomes, and the impact of nutritional supplements in adults with thalassemia were still unclear.
Objectives: To evaluate the prevalence of malnutrition and plasma metabolomic profiles of adult thalassemia when compared with healthy control, as well as to evaluate the effects of oral nutritional supplements (ONS) on nutritional status and metabolomic profiles in those thalassemia patients with malnutrition
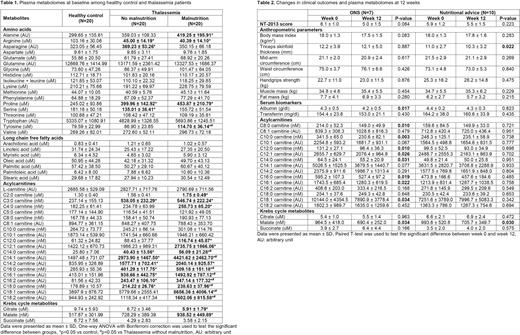
Methods: Adult thalassemia (n=100) and healthy control (n=20) aged ≥ 18 years old were enrolled in the present study. This study was divided into 2 phases. Phase I of the study: All participants were assessed nutritional status by nutrition assessment 2013 (NT-2013), serum biomarkers (albumin, transferrin), and anthropometry. Plasma metabolomes including amino acids, long-chain free fatty acids, acylcarnitines (C0-18), and Krebs cycle metabolites were measured by liquid chromatography-quadrupole time-of-flight mass spectrometry (LC/Q-TOF-MS). All outcomes were compared among 3 groups including thalassemia with malnutrition, thalassemia without malnutrition, and healthy control. Phase II of the study, thalassemia patients with malnutrition, defined as NT-2013 score of 5 or more, were randomized into two subgroups. Each subgroup received either ONS or nutritional advice by a nutritionist for 3 months. ONS consisted of oral complete formula (Blendera-MF®) and/or whey protein based on the assessment by food questionnaire to achieve the target of individual total daily energy expenditure (Harris-Benedict equation multiplied with activity factor) and total protein of 1.3 g/kg/day. NT-2013, anthropometric parameters, serum biomarkers, and plasma metabolomes were re-evaluated after 12 weeks in each subgroup. ONS adherence was assessed every 2 weeks during the study period. Those with less than 80% ONS adherence were excluded from the final analysis.
Results: A total of 100 patients were enrolled with a mean age of 34.9 years (range 18-60). Of which, 65.3% were females and 58.1% were transfusion-dependent thalassemia (TDT). The prevalence of malnutrition was 20% (15% mild, 85% moderate degree). Malnutrition was more common in TDT than non-TDT (30.9% vs 6.7%, p=0.003). Twenty age, sex, and body mass index-matched healthy controls were also enrolled. Regarding plasma amino acids, baseline alanine, proline, and tyrosine were significantly increased while arginine was significantly decreased in malnourished patients. Fatty acid-derived acylcarnitines (C12-18) were significantly increased in malnourished patients compared to the control group. Long-chain free fatty acids were not different between groups. Considering Krebs cycle, citrate was significantly decreased, but malate was significantly increased in malnourished patients compared to the control group (Table 1). Three participants had less than 80% ONS adherence. After 12 weeks, the mean NT-2013 score in overall malnourished patients significantly improved, when compared to their baseline (6.0±1.1 to 5.2±1.5, p=0.029). However, there was a trend of more improvement in ONS group than nutritional advice group (6.1±1.0 to 5.0±1.5, p=0.084 vs. 5.9±1.2 to 5.5±1.5, p=0.223). Fatty acid-derived acylcarnitines (C8-18) and malate were significantly decreased after ONS (Table 2). Anthropometric parameters, serum biomarkers, long-chain free fatty acids, and amino acids were not changed.
Conclusions: The prevalence of malnutrition in adult thalassemia was 20%. Plasma metabolomic profiles suggested that the malnourished thalassemia had imbalanced protein turnover and incomplete fatty acid oxidation, resulting in the disruption of Krebs' cycle. Among thalassemia patients with malnutrition, both ONS and nutritional advice led to improve nutritional status. ONS for 12 weeks also promoted more complete fatty acid oxidation in malnourished thalassemia.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal